Case Report: Squamous Cell Carcinoma, age 80, Female
Surgical biopsy, oral fenbendazole then topical fenbendazole eradicates squamous cell carcinoma
Fenbendazole Can Cure Cancer presents Case Reports of people who have treated their own cancers along with other articles to help understand how fenbendazole works to treat cancer. Previous articles covering other cancers are in the Archives link.
According to the Mayo Clinic, squamous cell carcinoma of the skin is a type of cancer that starts as a growth of cells on the skin, originating in cells called squamous cells. Squamous cell carcinoma is a common type of skin cancer. Squamous cell carcinoma of the skin is usually not life-threatening. But if it's not treated, squamous cell carcinoma of the skin can grow large or spread to other parts of the body.
Squamous cell carcinomas can appear anywhere on the skin. In people who sunburn easily, the cancer is usually found on areas of skin that have had a lot of sun. In people with black and brown skin, squamous cell carcinomas are more likely to be on skin that isn't exposed to sun, such as the genitals - which conflicts with the notion that topical UV radiation is the primary cause.
The following Case Report is submitted by the daughter of an 80-year-old woman who had a persistent lesion on one of her fingers. Initially diagnosed as a basal cell skin cancer that diagnosis was revised to squamous cell skin cancer after biopsy results. After about a 3 month course of systemic (oral) fenbendazole treatment, with a topical component added about one month into the treatment, the lesion is completely healed.
Hi Ben,
I've followed the Substack for a while and was curious enough to buy FenBen powder from the Lithuanian supplier
No one had cancer but I thought it would be good to at least use it as a dewormer and do a 3 day clean out of any parasites every few months. Hopefully, this would also provide some protective benefits from any cancers.
As "luck" would have it, my 80 year old mom was diagnosed with a basal cell carcinoma (later revised to squamous cell) of the finger.
For several years (she says about 4) the finger has bothered her. She thought it was an injury that wasn't healing well because it was in her knuckle. Combine that with thin ageing skin and she would regularly knock the sore open just as it seemed to be healing. Over the past year it had been getting infected on a regular basis. It would scab over, heal slightly but still be stiff and painful. A slight bump and it would burst open oozing yellow pus.
She saw her GP as no amount of bandaging and antiseptic lotion seemed to effect any healing.
Travacort and an oral fungicide were prescribed. No improvement.
They then dipped a swab and off the back of finding bacterial growth she was given a course of antibiotics. It almost seemed to worsen with a nasty open wound causing her tremendous pain in the finger joint.
She saw a nurse at the local hospital wound clinic who scraped it all clean, bandaged it up and strongly suggested she request her GP do a biopsy as “sores which don't heal over several years are suspicious”.
This was duly done and it proved to be a basal cell carcinoma (later revised to squamous cell).
The problem now was how to excise it. On a joint. No skin left to suture and she's 80 years old.
He said to leave it a couple of weeks as he was going to be away and he would give it some thought as to how to proceed but it would likely require in hospital treatment and anaesthesia to be able to do a skin graft.
This worried me greatly as mum is 80.
So I went over to her with the FenBen powder and told her she was going to be the family Guinea pig. At worse she'd be thoroughly dewormed and there might be some benefit.
I have attached 3 photos. The first is the sore on the day the biopsy was done. Call it Day 1 and you'll see the pus and raw nature of the sore.
Day 7. Looking vastly improved and she had no pain for the first time in over a year.
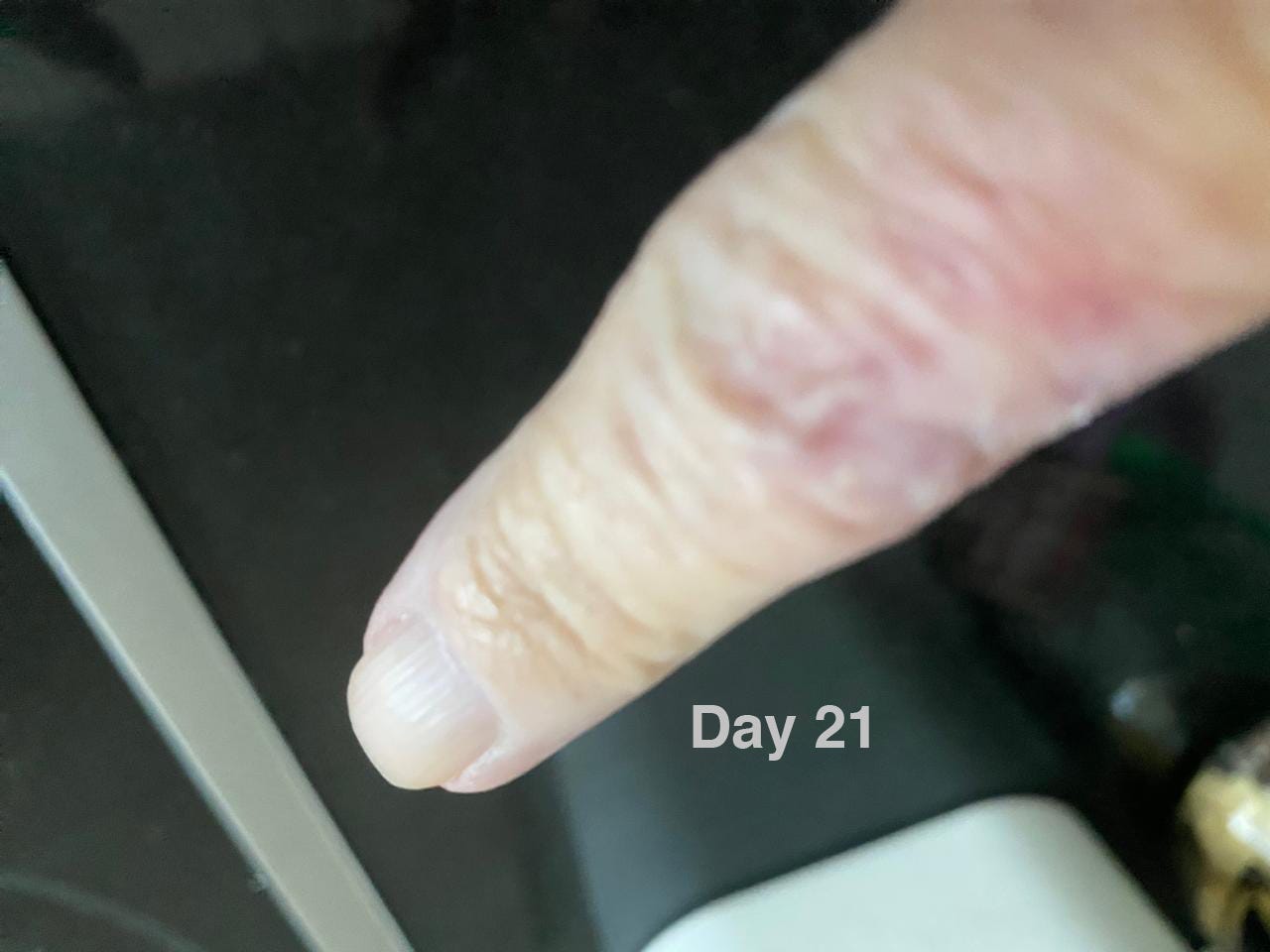
Day 21. The last photo is taken 3 weeks after the initial oral dose of powder. 222mg as dosed by the little spoon in the tub. Taken daily with cheese or something fatty.
As you can see, the skin has healed over. She has free use of the finger and there is no pain.
She's had no obvious side effects from taking the Fenben.
She's seeing her GP on Tuesday next week and I'm keen to hear what he says. Hopefully he won't mess with it and we can go back in a few months once the new skin has matured and do a follow up biopsy.
Hope this is interesting to you! She's not the best of photographers but there's clearly been a massive improvement. We are so grateful to you for posting these self studies!
Follow-up 5 weeks later
My mother saw her GP not long after I last emailed you and he seemed quite surprised to see how well the finger was doing and ascribed it to the fact that when he'd previously seen her, that he had cut some of it out when he sampled for the biopsy and put the stitches in. She mentioned the FenBen and said he was reluctant to believe that it had anything to do with it but he had to concede that it was looking very good and all plans to surgically remove the carcinoma and do a skin graft under general anaesthesia could be shelved. For now.... I suspect he thinks it will be back.
Since the wound had closed completely she has been applying FenBen paste topically every day (Panacur “horse dewormer”). She leaves her finger exposed to the sun and fresh air as much as possible, putting a plaster over when she goes out as she’s worried about knocking the new skin open after years of pain.
It continues to look good with no external signs of infection, no pain in the affected area or joint and the skin has healed beautifully. Really quite astonishing given how many years this carcinoma has had to eat away at the skin and being 80 it’s quite thin without any extra stresses on it.
Mom says she sometimes imagines there might be a small amount of the cancer left as she sometimes “feels” like there's “something” moving around under the skin but this is as likely to be residual deep tissue damage resolving itself as it is any cancer. She says it tingles sometimes but this really does seem more likely to be healing than cancer. The sutures she had a few months ago have also left a bit of lumpy skin. There’s no way she will biopsy the area to confirm if the cancer has gone, as there's just no obvious reason to traumatise healthy looking skin.
I've attached photos of the finger as of today. I'm not sure of where you are in the world but it's midwinter here so her skin does look a bit dry but that's the weather.
As far as we can see, there's no cancer left. She has had no obvious side effects from taking the FenBen and will continue with it both orally and with the topical cream. I bought her a milk thistle supplement but only because I read there could be effects on her liver and if she's been clearing the cancer it might be a good thing. Just me fussing there was no obvious reason to do so!
June 19, 2024
Mom went to see her GP today. He says he's not convinced the cancer is gone and wants to carry on with an excision off the back of the pathology report, which I have attached. Since he excised some of the carcinoma when he took the biopsy sample, he feels this is the reason for the improved appearance. I'm not so sure .... cancer sores don't get better as far as I'm aware!!
In any event, the full diagnosis is attached. Seems it’s a squamous cell carcinoma and there's also some signs of Bowen’s disease and solar elastosis.
We're about 2 months down the road treating a 4 year old tumour. At the age of 80, I honestly believe my mom should leave it alone and continue with the Fenben and just see where it goes. I find it hard to believe there's a festering tumor underneath all that healthy new skin as she has full use of the finger and has no pain at all. At any other point in time she would not be seeing a GP......
August 10, 2024
It's been 3 months now and my mom's finger seems to have healed completely since we last corresponded. In her words "If you didn’t know history you’d never guess".
A friend has had a squamous carcinoma diagnosed on his face and is keen to try FenBen. I'll guide him along same lines as my mom and let you know if ( when! ) it improves.September 27, 2024
Nice to hear from you. All good to publish. That finger is now so well she's started to forget applying the cream.
Mum has also read it and said the doctor made the comment that he "guaranteed" it would come back when he was advocating for the skin graft.
It's been at least a month since we last corresponded and that finger never looked better.Many thanks
Caroline
—- C. D., Johannesburg, South Africa, September 28, 2024
Q: How is your Mom doing now?
A: Good and 110% convinced the FenBen has cleared the cancer.
Q: Is your Mom continuing to take or apply fenben?
A: Yes. Although she seems asymptomatic she'll apply the cream topically and take 222mg a day for another 3 months. We've no real idea as to how long to treat her! If we do this, she will have had a total of 6 months on the powder and 4 months of topical application. (Recall the first two months, the finger had an open festering wound, often infected applying cream would possibly have been unwise).
After these 6 months, I’ll suggest she stop taking it daily, and move to the prophylaxis type dosing regime of 222mg daily for 3 days each month, possibly weaning her off it over a period by taking every 2 days, then 3 days, ....then weekly etc. Regarding preventing a recurrance this is what I've seen between extremes of taking the stuff ad infinitum and a cold stop. Once a month for 3 days seems as good a choice as any.
Summary
Congratulations to Caroline and her mother for taking an active role in dealing with her Mom’s persistent condition. This report is one of several demonstrating the therapeutic effect of fenbendazole on various skin cancers including melanoma, basal and squamous cell. It is also noteworthy that this report includes the topical application of fenbendazole as an effective route of administration.
General References
Bai RY, Staedtke V, Rudin CM, Bunz F, Riggins GJ. Effective treatment of diverse medulloblastoma models with mebendazole and its impact on tumor angiogenesis. NeuroOncology. 2015; 17:545-54.
Chiang RS, Syed AB, Wright JL, Montgomery B, Srinivas S. Fenbendazole enhancing anti-tumor effect: A case series. Clin. Oncol. Case Rep. 2021; 4:2.
Dobrosotskaya IY, Hammer GD, Schteingart DE, Maturen KE, Worden FP. Mebendazole monotherapy and long-term disease control in metastatic adrenocortical carcinoma. Endocr. Pract. 2011; 17(3):e59-e62.
Doudican NA, Byron AA, Pollock PM, Orlow SJ. XIAP downregulation accompanies mebendazole growth inhibition in melanoma xenografts. Anti-Cancer Drugs. 2013; 24:181-8.
Gallia GL, Holdhoff M, Brem H, Joshi AD, Hann CL, Bai RY, et al. Mebendazole and temozolomide in patients with newly diagnosed high-grade gliomas: results of a phase 1 clinical trial. Neuro- Oncology Advances. 2021; 3:1-8.
Guerini AE, Triggiani L, Maddalo M, Bonu ML, Frassine F, Baiguini A, Alghisi A. Mebendazole as a candidate for drug repurposing in oncology: An extensive review of current literature. Cancers. 2019; 11:1284.
Meco D, Attina G, Mastrangelo S, Navarra P, Ruggiero A. Emerging perspectives on the antiparasitic Mebendazole as a repurposed drug for the treatment of brain cancers. Int. J. Mol. Sci. 2023; 24:1334.
Nygren P, Larsson R. Drug repositioning from bench to bedside: tumor remission by the antihelmintic drug mebendazole in refractory metastatic colon cancer. Acta Oncol. 2014; 53(3):427-8.
Nygren P, Fryknas M, Agerup B, Larsson R. Repositioning of the anthelmintic drug mebendazole for the treatment for colon cancer. J. Cancer res. Clin. Oncol. 2013; 139:2133-40.
Pantziarka P, Bouche G, Meheus L, Sukhatme V, Sukhatme VP. Repurposing drugs in oncology (ReDO) - mebendazole as an anti-cancer agent. Ecancer. 2014; 8:443.
Patel, H., Yacoub, N., Mishra, R., White, A., Long, Y., Alanazi, S., & Garrett, J. T. (2020). Current Advances in the Treatment of BRAF-Mutant Melanoma. Cancers, 12(2), 482.
Pinto LC, Soares BM, de Jusus Viana Pinheiro J, Riggins GJ, Assumpcao PP, Burbano RM, Montenegro RC. The anthelmintic drug mebendazole inhibits growth, migration and invasion in gastric cancer cell model. Toxicology in Vitro. 2015; 29:2038-44.
Pinto LC, de Fatima Aquino Moreira-Nunes C, Soares BM, Rodriguez Burbano RM, de Lemos JA, Montenegro R. Mebendazole, an antiparasitic drug, inhibits drug transporters expression in preclinical model of gastric peritoneal carcinomatosis. Toxicology in Vitro. 2017; 43:87-91.
Sasaki JI, Ramesh R, Chada S, Gomyo Y, Roth JA, Mukhopadhyay T. The anthelmintic drug mebendazole induces mitotic arrest and apoptosis by depolymerizing tubulin in non-small cell lung cancer cells. Molecular Cancer Therapeutics. 2002; 2:1201-9.
Simbulan-Rosenthal CM, DDakshanamurthy S, Gaur A, Chen YS, Fang HB, Abdussamad M, et al. The repurposed anthelmintic mebendazole in combination with trametinib suppresses refractory NRASQ61k melanoma. Oncotarget. 2017; 8:12576-95.
Tan Z, Chen L, Zhang S. Comprehensive modeling and discovery of mebendazole as a novel TRAF2- and NCK-interacting kinase inhibitor. Scientific Reports. 2016; 6:33534.
Walk-Vorderwulbecke V, Pearce K, Brooks T, Hubank M, Zwaan cM, Edwards AD, Ancliff P. Targeting acute myeloid leukemia by drug-induced c-MYB degradation. Leukemia. 2018; 32:882- 9.
Items Included in All Posts
Fenbendazole vs. Mebendazole vs. Albendazole vs. Flubendazole: The benzimidazoles are very similar chemically and they have very similar mechanisms of action with respect to disrupting microtubule function, specifically defined as binding to the colchicine-sensitive site of the beta subunit of helminithic (parasite) tubulin thereby disrupting binding of that beta unit with the alpha unit of tubulin which blocks intracellular transport and glucose absorption (Guerini et al., 2019). If someone asks you how fenbendazole kills the cancer cells, the answer is in italics in the previous sentence.
The class of drugs known as benzimidazoles includes fenbendazole, mebendazole, albendazole and flubendazole. Mebendazole is the form that is approved for human use while fenbendazole is approved for veterinary use. The main difference is the cost. Mebendazole is expensive ~$555 per 100 mg pill, while fenbendazole is inexpensive ~48 cents per 222 mg free powder dose (Williams, 2019). As you may recall, albendazole is the form used to treat intestinal parasites in India and these cost 2 cents per pill. FYI, to illustrate how Americans are screwed by Big Pharma, two pills of mebendazole cost just $4 in the UK, 27 cents per 100 mg pill in India and $555 per 100 mg pill in the US.
While most of the pre-clinical research uses mebendazole, probably because it is the FDA-approved-for-humans form of fenbendazole, virtually all of the self-treating clinical reports involve the use of fenbendazole. Because the pre-clinical cancer studies use mebendazole (ironically the human form of fenbendazole) and humans self-treat their cancers with fenbendazole (the animal form of mebendazole) it is very reasonable to assume that mebendazole and fenbendazole are functional equivalents with respect to cancer. It would be helpful if future pre-clinical and clinical investigations simply used fenbendazole as a practical matter. For the purposes of this Substack, fenbendazole, mebendazole and albendazole are used interchangably.
Where to get fenbendazole
In our experience and the experiences of those that write in, it appears that the three readily available brands of fenbendazole (Panacur-C, FenBen Labs, Happy Healing Labs) are equally effective. Panacur-C can be obtained locally in pet stores, while they all can be obtained from Amazon. The article on Questions & Answers discusses the brands of fenbendazole in detail and shows photos of the various brands referenced.
If you would like to report your experiences with fenbendazole you can do so privately by email myfenbendazole@proton.me or more publicly in the Comments section in any of the articles. Also, if you know of people who’ve tried fenbendazole, and it didn’t work, we’d be especially interested in hearing from you now. Understanding the conditions and factors that enhance or impede the success of fenbendazole in treating cancer are valuable.
Disclaimer:
Statements on this website have not been evaluated by the Food and Drug Administration. The contents of this website is for educational and informational purposes only and is not intended to be a substitute for professional medical advice, diagnosis or treatment. This website does not provide any kind of health or medical advice of any kind. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. The case reports presented reflect the real-life experiences and opinions of other readers or users of the website. The experiences of those readers or users are personal to those particular readers/users and may not necessarily be representative of all readers/users. We do not claim, and you should not assume, that all other readers/users will have the same experiences. Do you own research, consult with relevant medical professionals before attempting to self-treat for any condition.









Very interesting report! It certainly appears the Fenben was what changed things to vast improvement and a probable cure. I would not allow any surgical treatment unless there was at least some minimal sign of recurrence, if it were me. Great to hear from you guys again!
BTW, since I last communicated with you guys regarding my much improved(but not quite NED) stage 4 prostate cancer, I had a new scan, this time using the much more sensitive PSMA scan. Far more likely to pick up something than the bone and CT scans I was diagnosed with almost 3 years ago. In fact, that made me a little nervous.
But for all practical purposes, this most sensitive scan showed nothing. None of the previous and larger lesions on my spine and arm were even mentioned. (lymph nodes had long since ceased to be an issue, and all soft tissue was still zilch). They found 1 "new" lesion on my cervical/thoracic spine. It is either a new lesion or was too small to be detected with the less sensitive scans. The radiologist said "might be a new neoplasm, might be arthritis". (and I do have arthritis in my neck). ............................... The "new"lesion had an "SUV" number of 5. I looked up these numbers, and the consensus seemed to be that 8 or 9 was the minimum for clinically meaningful cancer. More importantly, the median for actual metastases was about 40 or so, with a range of about 25 to 75. So, at 5, if this is indeed a met from my metastasized prostate cancer, it sure is low on the scale.
I'm calling this "NED" until proven otherwise. My PSA remains undetectable for almost 3 years now. It became undetectable within 30 days of starting with the prescribed testosterone blockers(Orgovix + Erleada) PLUS my own DIY repurposed drug cocktail. To which FenBen was added about 11 months ago now. I still take the FenBen, and will for a while, but not as often. Now if I can just get off of those prescribed drugs!
I suggest taking fenbendazole with another great cancer fighter, Artemisinin.
Personally... IF I had cancer... I would also add Ivermectin to the mix.