Case Report: Desmoid Tumor (Aggressive Fibromatosis), age 34, Male
Fenbendazole Eradicates Non-Cancerous Tumor After Other Treatments Fail
Fenbendazole Can Cure Cancer presents Case Reports of people who have treated their own cancers along with other articles to help understand how fenbendazole works. Previous articles covering other cancers are in the Archives link.
According to the Mayo Clinic, desmoid tumors are noncancerous growths that occur in the connective tissue. Desmoid tumors most often occur in the abdomen, arms and legs. Another term for desmoid tumors is aggressive fibromatosis.
Some desmoid tumors are slow growing and don't require immediate treatment. Others grow quickly and are treated with surgery, radiation therapy, chemotherapy or other drugs.
Desmoid tumors aren't considered cancers because they don't spread to other areas of the body. But they can be very aggressive, acting more like cancers and growing into nearby structures and organs. For this reason, people with desmoid tumors are often cared for by cancer doctors.
Case Report
The following is a detailed Case Report of a man with an aggressive desmoid tumor and his experience in using fenbendazole to eradicate that tumor as told by his wife.
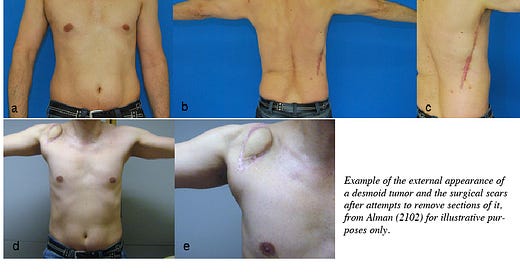
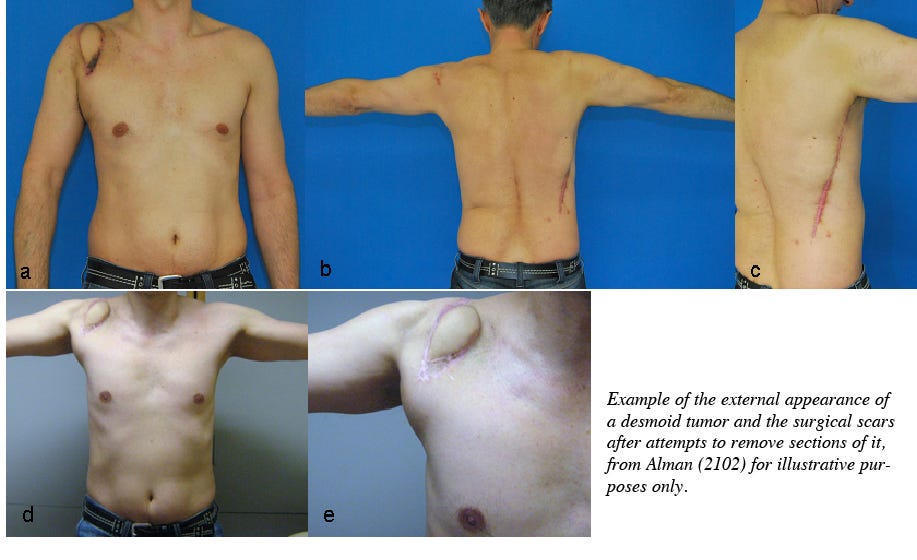
34 year old man with aggressive fibromatosis (desmoid tumor) on his left shoulder/scapula extending into his chest wall. This is a non-metastasizing tumor but is treated as a sarcoma due to its rapid, aggressive growth, and its ability to spread into large muscle groups (or the abdomen). This can be deadly, and almost always disfiguring.
2017 - My husband had a surgery to remove a lipoma on the left scapular area (same general area where the desmoid tumor eventually shows up)
April 2018 - He injured his left shoulder and shortly after he noticed a new mass in the same area. It is believed that fibromatosis may be the uncontrolled overgrowth of scar tissue and can be triggered by injury.
October 2018 - He underwent an MRI, biopsy and other diagnostic tests and was told it was fibromatosis. It was relatively small at this time (3cm x 1.4cm x 1.3cm).
November 2018 - He underwent surgery to remove the tumor. His doctor was confident that he got it all out (the microscopic margins were clean) and he had to remove an entire muscle from his shoulder in the process. Because of the muscle removal he was supposed to be unable to move his left arm in a certain direction but with exercise and work he overcame that boundary and surprised his doctor :)
July 2019 - The tumor began to grow back but they just kept monitoring it with frequent MRI’s.
January 2020 - The tumor had grown over twice the size that it was originally and chemotherapy was started (sorafenib). He took this for a year.
November 2020 - He also tried cryoablation treatment as well on multiple sites. At this point the tumor had become very aggressive and had grown very long and had extended into multiple ribs (causing non-displaced rib fractures), his chest wall, scapula and the pleural membranes surrounding the lungs. The chemotherapy kept it from growing but that was all. After several cryoablation treatments it did shrink it a bit but didn’t go away (it went from 16cm x 6cm x 3cm to 5cm x 3cm x 5cm). He also ended up with a brachial plexus injury resulting from the last cryo procedure (3/2021) and was unable to use his left arm.
September 2021 - The tumor had already grown over twice its size again. And here’s where fenbendazole comes in. I learned about fenbendazole when my dog was diagnosed with lymphoma in June 2021, his story was also posted on here (Moose). He’s still doing just fine, no evidence of reoccurrence. Now he’s just a happy, albeit lazy old dog who is enjoying his retirement.
November 2021 - He decided to have one more surgery which removed as much as they could but not all, and followed it up with radiation treatment immediately afterwards for about a month.
November 2021 - He started fenbendazole as soon as he began radiation therapy. He took 222 mg daily (Fenben brand from the Happy Healing Store).
May 2022 - His next MRI still showed enhancement but it was likely scarring from treatments, etc.
December 2022 - MRI showed fluid collection only, likely related to radiation therapy, but no tumor.
June 2023 - MRI showed no evidence of disease.
He has spoken with many others with these tumors and they do not experience such an outcome. Many are disfigured by multiple drastic surgeries, have desperately tried multiple treatments to no avail, and many have died. The abdominal form of this disease is the most deadly because of its invasion into the larger blood vessels. My husband is the only one who has had a positive outcome and the only thing he has done differently is taken fenbendazole.
————————————————
A. S., Winchester, VA July, 15, 2023
Q: It looks like that the timeframe was about a year until the tumor was gone (after starting fenbendazole), but that you suspect it may have been largely gone at 6 months...the first assessment after fenben was started?
A: He is now 40 years old, the tumor was diagnosed when he was 34 years old, I guess that sort of paints a pretty good picture of the long and difficult journey this has been trying to overcome this. Up until a year after radiation/fenben treatment, they wouldn’t say “no evidence of disease”. There was some enhancement but we were told it was edema and likely scar tissue resulting from surgery/radiation. On his most recent scan, they actually did finally say “no evidence of disease”. I believe the fenbendazole worked within the first 6 months especially because his tumor was so diffuse and widespread, they were not able to access it, in its entirety, with neither surgery nor radiation.
Q: Did the doctor(s) know your husband was taking fenben? Did they have any comments?
A: He didn’t tell his oncologist until his most recent appointment in June. His doctor was intrigued and was just happy that he was finally tumor free.
Q: One last question: did he take any supporting substances like vitamin E, CBD oil, etc. that some associate with the effectiveness of fenbendazole?
A: He also took sweet wormwood, multivitamin, vitamin D3/K2, krill, bee propolis, magnesium.
Summary
Congratulations to this couple for thinking outside the box, taking control of a difficult situation, and making a potentially huge discovery in the process. Eradicating a tenacious tumor like this, that wraps itself around other structures making its complete removal almost impossible, is a remarkable feat.
Why is this a potentially interesting discovery? In addition to identifying that fenbendazole is effective on desmoid tumors and potentially saving yet more heartache and lives, fenbendazole’s effectiveness on this “non-cancerous” growth is remarkable in other ways as well. It shines a spotlight on how we conceptualize what we consider cancerous growths, perhaps leading to a better understanding of how we can eradicate them.
Is cancer conceptually much simpler than it appears? Have we overthought the complexity of cancer such that the obvious has been overlooked? Is cancer simply a “parasite” that shares similar structural vulnerabilities to other parasites, like the parasitic worm’s microtubule system affected by fenbendazole? Since it appears that non-cancerous desmoid tumors are similarly eradicated by fenbendazole, the category on which fenbendazole acts is broader than that of just “cancer” and/or “parasites”.
Consider the following:
• Invasive worms are not cancerous but their behavior is parasitic. They are eradicated by fenbendazole, an antiparasitic.
• Desmoid tumor cells are not cancerous but their behavior is parasitic. These cells, too, are eradicated by fenbendazole.
• Cancer cells should be considered parasitic because their behavior is such, and they are eradicated by fenbendazole.
The host of diseases that we label collectively as cancer may be better characterized as parasitic infections. (Cancer viewed as a parasite is conceptually different to prior theories of cancer being caused by parasites, see Plimmer (1903), yes 1903!) It is not unreasonable to conclude that cancer is better characterized as a parasite based on its behavior as well as its selective susceptability to eradication by the antiparasitic medicine fenbendazole.
Why does it matter how we conceptualize cancer? Because how we think about something determines the approach we will take towards dealing with it. Contemporary approaches to cancer research view the cells we call cancer as primarily a result of genetic malfunction or metabolic malfunction (Wishart, 2015). If we only look for genetic causes and therapies, and metabolic causes and therapies, guess what? We only find those causes and treatments! Think about it this way: if all one has in their toolbox is a hammer, everything tends to look like a nail. Which accounts for the less than perfect results from oncological research over the past 100+ years. Less than perfect because, while a hammer can be used for other tasks, it does them inefficiently, sloppily and perhaps detrimentally, causing more harm than good in the long run. More on this topic in future issues.
Recharacterizing, or thinking about cancer as a potential parasite opens up the possibility of widespread acceptance of that fact that the antiparasitic medicine Fenbendazole Can Cure Cancer.
References
Alman, B. (2012). Desmoid Tumors: Are They Benign or Malignant?. In: Litchman, C. (eds) Desmoid Tumors. Springer, Dordrecht. https://doi.org/10.1007/978-94-007-1685-8_13
Plimmer H. G. (1903). THE PARASITIC THEORY OF CANCER. British Medical Journal, 2(2241), 1511–1515. https://doi.org/10.1136/bmj.2.2241.1511.
Wishart, D. S. (2015). Is Cancer a Genetic Disease or a Metabolic Disease? eBioMedicine, 2, 478-479. https://doi.org/10.1016/j.ebiom.2015.05.022
Fenbendazole vs. Mebendazole vs. Albendazole vs. Flubendazole: The benzimidazoles are very similar chemically and they have very similar mechanisms of action with respect to disrupting microtubule function, specifically defined as binding to the colchicine-sensitive site of the beta subunit of helminithic (parasite) tubulin thereby disrupting binding of that beta unit with the alpha unit of tubulin which blocks intracellular transport and glucose absorption (Guerini et al., 2019). If someone asks you how fenbendazole kills the cancer cells, the answer is in italics in the previous sentence.
The class of drugs known as benzimidazoles includes fenbendazole, mebendazole, albendazole and flubendazole. Mebendazole is the form that is approved for human use while fenbendazole is approved for veterinary use. The main difference is the cost. Mebendazole is expensive ~$555 per 100 mg pill, while fenbendazole is inexpensive ~48 cents per 222 mg free powder dose (Williams, 2019). As you may recall, albendazole is the form used to treat intestinal parasites in India and these cost 2 cents per pill. FYI, to illustrate how Americans are screwed by Big Pharma, two pills of mebendazole cost just $4 in the UK, 27 cents per 100 mg pill in India and $555 per 100 mg pill in the US.
While most of the pre-clinical research uses mebendazole, probably because it is the FDA-approved-for-humans form of fenbendazole, virtually all of the self-treating clinical reports involve the use of fenbendazole. Because the preclinical cancer studies use mebendazole (ironically the human form of fenbendazole) and humans self-treat their cancers with fenbendazole (the animal form of mebendazole) it is very reasonable to assume that mebendazole and fenbendazole are functional equivalents with respect to cancer. It would be helpful if future pre-clinical and clinical investigations simply used fenbendazole as a practical matter. For the purposes of this Substack, fenbendazole, mebendazole and albendazole are used interchangably.
Where to get fenbendazole
In our experience and the experiences of those that write in, it appears that the three readily available brands of fenbendazole (Panacur-C, FenBen Labs, Happy Healing Labs) are equally effective. Panacur-C can be obtained locally in pet stores, while they all can be obtained from Amazon.
If you would like to report your experiences with fenbendazole you can do so privately by email fenbendazole77@gmail.com or more publically in the Comments section in any of the articles. Also, if you know of people who’ve tried fenbendazole, and it didn’t work, we’d be especially interested in hearing from you now. Understanding the conditions and factors that enhance or impede the success of fenbendazole in treating cancer are valuable. As an example, we recently learned that pairing fenbendazole with oleic acid (olive oil has high oleic acid content) greatly enhances the bioavailability of fenbendazole (Liu et al., 2012). As a practical application of this information taking fenbendazole with a tablespoon of olive oil may result in better outcomes.
Disclaimer:
Statements on this website have not been evaluated by the Food and Drug Administration. The contents of this website is for educational and informational purposes only and is not intended to be a substitute for professional medical advice, diagnosis or treatment. This website does not provide any kind of health or medical advice of any kind. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. The case reports presented reflect the real-life experiences and opinions of other readers or users of the website. The experiences of those readers or users are personal to those particular readers/users and may not necessarily be representative of all readers/users. We do not claim, and you should not assume, that all other readers/users will have the same experiences. Do you own research, consult with relevant medical professionals before attempting to self-treat for any condition.




If anyone is so inclined, we'd like some feedback on the proposal that cancer behaves like a parasite, and is most likely a parasite because an antiparasitic medicine eradicates it. Especially observations that are contrary to the idea. Seems too simplistic at first blush but we're at a loss for evidence to dismiss the idea.
I have probably 6-7 of your case studies now. I got to say looks very promising. I have 4 friends right now since Covid started that have been diagnosed with stg 4 colon, stg 3-4 metastasized breast cancer, pancreatic cancer. I sent all of them these studies, because what do they have to lose , right? They all agreed to read them. I told them take what you want and leave the rest. It is now in their hands. But I couldn’t not send these case studies not when they’re facing stages 3-4 in Cancer. Thank you for putting these out there.